The First Day
Feeding Starts at Birth
The best time to start breastfeeding is right after birth, if you and your baby are both stable. Ask for your baby to be placed skin-to-skin on your body, with a baby blanket over the two of you, as soon as possible after birth and before the baby is bathed.
Benefits of skin-to-skin contact:
- Helps stabilize baby’s body temperature, blood sugar, heart rate, and breathing
- Increases baby’s feelings of safety and security
- Stimulates baby’s feeding reflexes
- Increases parent’s milk supply earlier
- Releases of the hormone oxytocin in the nursing couple

The Breast Crawl
When placed skin-to-skin, many babies will soon move to the breast by themselves and latch onto the nipple. This is known as the “breast crawl.” The baby should be left skin-to-skin on the birth parent for the first hour after birth or until the first feeding is completed. Weighing and measuring the baby and other birth procedures can take place after the feeding.
Colostrum – The Special First Milk
During later pregnancy and immediately after birth, the breasts contain a special first milk known as colostrum, which is yellow or clear. Colostrum is the perfect first food for babies because it is:
- High in protein and antioxidants
- Rich in antibodies and other factors that protect the baby from illness
- Helps the baby pass their first stools

If the baby does not latch to the breast, the parent can hand express colostrum from the breast directly into the baby’s mouth or onto a spoon to provide the first feeding to the baby. Newborn babies’ stomachs are tiny and they only need about a teaspoon (3-7 ml) of colostrum at their first feeding. Ask the doctor, midwife or the nurses at your birth for assistance with hand expression if you need it.
Rooming In
When ready, you and baby can be moved from the delivery room to the patient room where you can remain together. This is known as “rooming in”. Keeping the baby in the same room with you will allow you to learn the baby’s feeding cues and get feeding off to a strong start.
Baby’s Hunger Cues
The baby should feed at least 8 times or every 2-3 hours or whenever the baby shows hunger cues. Babies show they are hungry by doing some or all of the following:
- Waking
- Hand-to-mouth movements
- Turning head side to side and opening mouth wide (rooting)
- Fussing or crying
If the baby is not self-waking every 2-3 hours, you should wake the baby and offer a feeding at the breast or chest. If the baby is having difficulty feeding during the first 24 hours, you can continue to feed hand expressed colostrum to the baby all day. Many mothers find they obtain more colostrum by using hand expression than by using a pump. Babies do not need a lot of food the first day, just about a teaspoon of colostrum every 2-3 hours or at least 8 times the first day. Rest as much as you can between feedings on the first day. It’s important to nap whenever possible, especially if you had a long birth.
How to Position Your Baby
There's no one right way to hold your baby while breastfeeding. Try different positions to see which ones work best for you and your baby. The best position is one that makes you and your baby comfortable and allows your baby to get a deep and comfortable latch!
Laid-back Breastfeeding
- Start by leaning back on your bed or couch into a semi-reclined position with your back and head supported by pillows or cushions as needed.
- Place your baby tummy to tummy on your body so their head rests near your breast. Baby will use hands, cheeks and nose to find the nipple.
- Relax and wait for your baby to latch, using gentle movements to help baby as needed.
- You can support your baby’s head and body with your arm so that you are both comfortable.

Cradle Hold
- Start sitting in an upright position on a comfortable chair using pillows for your own comfort.
- Place your baby tummy-to-tummy with you across your front. Baby's head will lay in the bend of your elbow, with baby's nose pointing to your nipple. Use a pillow under baby if necessary to support the baby and your arm.
- Use your opposite hand to support the breast while baby is latching if necessary.
- Use the rest of your arm to support the rest of your baby’s body and bottom. Use that arm to keep baby's body right next to your body.
Cross Cradle Hold
- Start in an upright position, using pillows behind your back and under the baby, if necessary, for comfort and positioning.
- Place your baby tummy-to-tummy across your body using your arm opposite from the breast you’re feeding from. Place baby so that his nose is opposite your nipple.
- Support your baby's head by making a U-shape with your thumb on one side and other fingers on the other. Place your U-shaped hand at the back of the baby's neck. The palm of your hand should rest against the baby's shoulder blades.
- Your arm can be wrapped around the back of the baby's body.
- Your other hand can be used to support your breast from the underside.
- When your baby feels the nipple and opens wide, bring the baby's body in closer to you by gently pushing with the palm of your hand between the baby's shoulder blades for a deep latch.


Football or Clutch Hold
- This position is helpful if you have had a C-section.
- Use a pillow alongside your body to support the baby. You can also tuck a pillow behind your back for comfort. Positioning that pillow away from baby's legs will give the baby good leg room.
- Hold your baby, facing up, under the breast that you are feeding from. Use a pillow underneath the baby to bring the baby's face and body to the level of your breast.
- Support your baby's head by making a U-shape with your thumb on one side and other fingers on the other. Place your U-shaped hand at the back of the baby's neck. The palm of your hand should rest against the baby's shoulder blades. The rest of your arm can rest alongside the baby's body.
- While the baby is latching, it can be helpful to use your free hand to support your breast and to point your nipple to baby's nose.
Side-lying Position
- Lie on your side. Use a pillow to support your head. Use more pillows behind your back or between your knees if needed.
- Place your baby on her side facing you, with her nipple near your nose. Flexing your baby at the hips and keeping his ear, shoulder and hips in a line can help.
- Use either arm to bring the baby in close your breast, if necessary. Use a pillow or rolled up blanket behind baby's back to keep the baby near you if necessary.
- This position can be comfortable and restful during the early days while your body is recovering from birth.

Getting a Deep Latch
Getting a comfortable, deep latch during feedings helps to ensure that the baby will get enough to eat and to prevent sore nipples. Nursing is not supposed to be painful. In a reclining, leaned-back position and with the baby skin-to-skin on your body, many babies will naturally use your body as support to help get a deep latch.
If your baby needs more help with deep latching, try these steps:
- In any position, start your baby positioned with his/her whole body facing your body, with the baby’s chin touching the breast below the nipple and with your nipple pointing up under the baby’s nose.
- Wait for baby to tilt his/her head back and open their mouth wide like a yawn.
- When baby’s mouth is open wide and your nipple is pointing to the roof of baby’s mouth, bring baby’s body in closer to yours by gently pushing baby behind the shoulder blades toward you. Baby will scoop up a big mouthful of the breast.
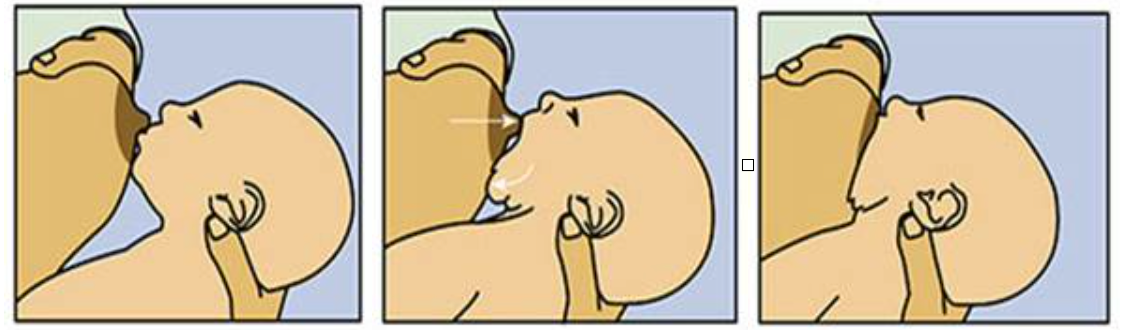
A deep latch should feel generally comfortable. If you feel pain after the first few seconds of sucking, put your finger into the corner of the baby’s mouth to unlatch the baby and try again.
Notify your nurse and the lactation consultant at your birth facility and ask for a lactation consultation if feeding difficulties continue.
Hormones at Work
You may feel some uterine cramping during feedings. This feeling is normal and common during the first 2-3 days. The cramping is caused by a release of the hormone oxytocin from your baby’s sucking. These “afterpains” are pulling your uterus back to its normal size. When your baby latches and begins to suck, oxytocin sends a message to your brain. The brain then signals another hormone, prolactin, to be released. Prolactin causes the milk sacs to make milk. Oxytocin causes muscles around the sacs to squeeze milk out to the nipple. When this happens, you may notice a tingling feeling in your breasts and at other times during the feeding, too.
The Second Day
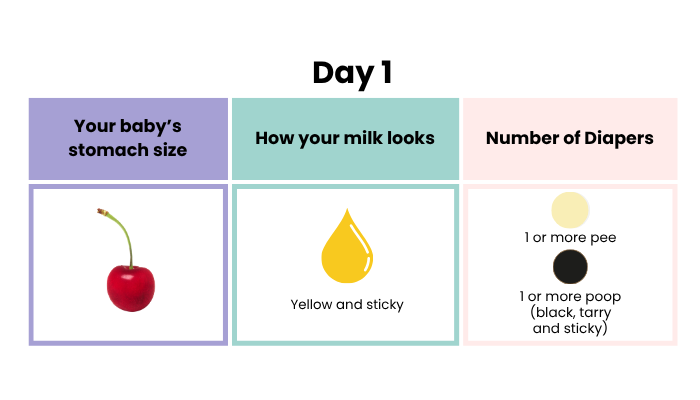
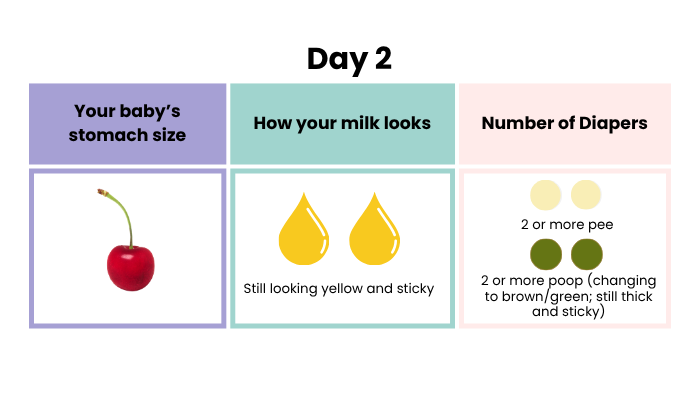
On the second day after birth, many babies are more alert and wake up more often to feed than they were on day 1. They want to get to know you and learn how to feed well. In the beginning, babies do not need much to fill their bellies. On Day 1-2, a baby’s stomach is about the size of a cherry. Your milk is still mostly colostrum, and your breasts probably still feel soft.
Cluster Feeding
Babies may also begin to “cluster feed” or feed almost every hour during part of the day. After several feedings close together, the baby will usually fall fast asleep for a few hours.
Cluster feeding is normal in early breastfeeding. The small, frequent cluster feedings are perfect for the baby’s small tummy and give plenty of feeding practice. Frequent feedings also tell your body to increase your milk supply to meet the baby’s needs and to change from colostrum to whiter, mature milk. The more the baby sucks, the more milk you make!
It is normal for the baby to feed 8-12 times in the second 24 hours after birth. Because of this frequency, it remains important to rest and take care of yourself between feedings. Some babies like to feed more at night than during the day, so resting during the day will help you to be prepared for that!

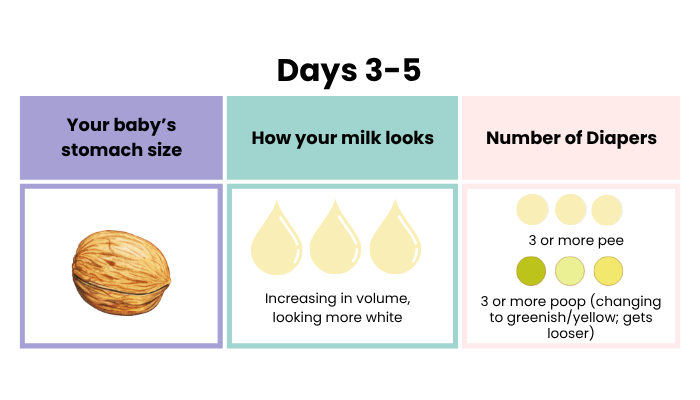
Days 3 -5
Changes in Milk Supply
Your breasts become bigger and heavier on days 3-5. That is when the milk supply increases and your milk changes from colostrum and becomes whiter, more like cow’s milk. The body also sends extra fluids to the area to help make more milk. During this time, keep feeding at least every 2-3 hours or more based upon baby's feeding cues to keep baby satisfied and your breasts comfortable.
For some parents, the breasts may become very large and hard at this time. This is called engorgement, and it is temporary. You can treat engorgement by:
- Continuing normal breastfeeding and avoiding any extra feeding or pumping
- Rest often lying on back if possible
- Apply ice for 20-30 minutes at a time between feedings
- Take Tylenol (acetaminophen) or Advil (ibuprofen) according to package instructions if recommended by your health care provider
These measures will help engorgement improve within 24-48 hours. At the same time, your breasts will adjust to making the amount of milk that your baby needs. Your breasts will feel full between feedings, but then softer after the baby feeds.
Signs Baby is Getting Enough to Eat
As your milk supply increases, the baby’s stomach also expands and can hold more milk by the end of the first week. You can know that your baby is getting enough to eat by making sure that baby is eating 8-12 times in 24 hours and by making sure that your baby is making at least the number of wet diapers shown in the chart below. Your baby should also be seen by a midwife, pediatrician or family physician within 3-5 days of being born or 1-3 days after leaving the birth facility.
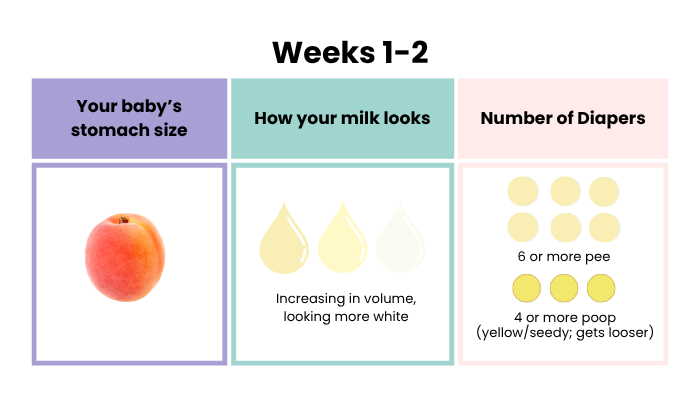
Weeks 1-2
Congratulations on making it through the first 5 days - you are on your way! You and your baby are getting to know each other better each day. Your baby’s stomach is growing to about the size of an apricot (see below). Your milk supply is also increasing every day to meet baby’s needs as you feed frequently.
Feedings
You may find that no two feedings are alike. For some feedings, baby may settle more easily into a long meal. At others, she may want to eat in a series of snacks. Many babies are still sleepier during the day and more alert at night at this stage. Your baby knows their nights from their days, but they may still prefer to learn how to feed well in the quiet darkness at midnight rather than during the bright, noisier daytime hours.
Breasts
Any engorgement experienced during days 3-5, should be improved. (If not, repeat engorgement management steps above.) You may notice that your breasts are fuller in the early morning and softer in the late day. Don’t worry about the evening. There’s still milk there, and it’s higher is certain hormones that will help the baby sleep.
Your Feelings and Emotions
Especially if this is your first time breastfeeding, you may wonder how this experience will go. You may feel disoriented by the baby’s lack of any consistent feeding and sleeping schedule. You may sometimes be unsure if the baby is hungry or has gas or is tired or overstimulated. Remember, babies are still getting used to life on the outside, and the only way they can tell you that something is not right is to cry. If you are unsure if your baby's crying is due to hunger, offer a breastfeeding anyway. Sucking and feeding can help calm the baby, move the gas, and make baby feel settled and ready for a nap. If that doesn’t work, you or a helper can hold and walk or rock the baby. Baby will feel better just being held.
You will need to be held sometimes, too, because you may feel a range of emotions. Initial amazement after giving birth may turn to self-doubt, weepiness, anxiety, and feeling overwhelmed. Giving birth causes a natural hormonal shift which can cause these mood changes known as the "baby blues". These feelings are common during at first, but they typically improve on their own by about 2 weeks. If you feel more than the baby blues or if your moods are not improving, consult the Beyond the Baby Blues section below
Exhaustion
You won’t be sleeping for long stretches in the early weeks, but that does not mean you can’t get enough sleep in 24 hours. Remember: You need to sleep when the baby sleeps. That means taking daytime naps or even just resting if you aren’t a natural napper. The good news is that the hormones of breastfeeding are calming and can help you nap easier and return to sleep faster after nighttime feedings.
First Two Weeks Checklist
- Offer baby the breast when the baby shows early signs of hunger (waking, opening mouth, turning head side-to-side, hand to mouth, rooting)
- Avoid pacifiers and bottles (unless you are feeding your baby pumped milk or must supplement breastfeeding)
- Look for signs that your baby is swallowing and making enough wet and soiled diapers (see diaper chart below).
- Sleep when the baby sleeps
- Keep visitors at a minimum unless they are very helpful to you (for example, cooking, cleaning, doing laundry and rocking the baby when you need to nap)!
- Drink to thirst and do your best to eat balanced meals plus healthy snacks when you can’t sit down to a meal and ask others to help with meals and grocery shopping
- Ask for emotional support from partners, family and friends during this period of recovery and change
- Take your baby to the 2-week well baby visit
Weeks 2-6
Every day with your newborn is still new and different as you both adjust to this new life together. You probably are not feeling like a feeding and childcare expert yet, but with more practice, you will likely see your baby make progress toward better feeding. If you are feeling breastfeeding pain that's not improving or have concerns about your baby's feedings, growth or diaper output, reach out to skilled lactation support. Find it on the
Get Help page.
| Day | # of Diapers /Color | # of Stools | Stool Color & Consistency |
|---|---|---|---|
| 1 | 1/pale yellow | 1 | Black, tarry, sticky |
| 2 | 2-3/pale yellow | 2 | Green/black, changing |
| 3-4 | 3-4/pale yellow | At least 3 | Green/yellow, soft |
| 4 | 4-6/pale yellow | At least 3 | Yellow/seedy, soft/liquidy |
| 5-30 days | 6+/pale yellow | At least 4 | Yellow/seedy, soft, liquidy |
| 31+ days | 6+/pale yellow | May slow down to 1 everyday or every few days | Yellow/seedy, soft, liquidy |
Feedings
Baby may be a little less sleepy and more business-like about feedings. As lactation consultant and author Nancy Mohrbacher says, your baby may start to develop more of a rhythm than a schedule by the end of this period. At around 3 and 6 weeks, your baby may seem to want to nurse constantly for a period of 2-3 days in a row. These are known as “growth spurts” and will settle down shortly. As long as you see sufficient wet and dirty diapers, this is normal. Your baby’s sucking will bring your milk supply up to the next level to meet growth needs.
Breasts
At around 3 weeks, you may notice that your breasts feel noticeably softer than they felt earlier, and you may worry that your milk supply is dropping. It’s common at this time for your breasts to synch to your baby’s needs to contain all the milk you need minus the swelling you had in the first 2 weeks. As long as your baby’s diapers are normal, there’s no need to worry.
Your Feelings
At this point, you may still feel you are struggling to meet all the baby’s needs and your own. Give yourself grace. Remember, there is no training program on earth that could have prepared you before the baby for the experience of parenthood. You must learn on the job. Keep reaching out to loved ones for help and support. Before long you will start to feel that you are getting better at your new role. If you are feeling depressed, sad, and anxious and not like yourself, see the Beyond the Baby Blues section below.
Beyond the Baby Blues: Postpartum Mood and Anxiety Disorders
Baby blues are common in the first two weeks after birth. However, if these feelings don’t go away after 2 weeks, you might be experiencing a perinatal mood and anxiety disorder (PMAD). The signs and symptoms can vary and may include:
- Excessive crying
- Irritability, anger, or rage
- Constant worry or anxiety
- Loss of interest in things you used to enjoy
If these symptoms last longer than two weeks or interfere with your ability to enjoy life and care for your baby, seek help from a health care professional. Call 988 immediately if you are having thoughts of harming yourself or others.
More resources on postpartum mood and anxiety disorders:
- Contact the New Jersey Postpartum Resources and Support Network for each region of the state:
- Central Jersey Family Health Consortium (for Central NJ residents)
- Partnership for Maternal and Child Health of Northern NJ (for North Jersey residents)
- The Cooperative (for South Jersey residents)
- Postpartum Support International
- Maternal Mental Health Hotline: 1-833-852-6262






